Rapid screening and diagnosis of active respiratory infections has emerged as a critical unmet need in improving patient outcomes and preserving public health. Hospitals need to know which infectious organisms are being carried in by new patients so that proper quarantines can be established. Once in the hospital, sick patients are often placed on antibiotics empirically due to a lack of fast, accurate, non-invasive diagnostic tests. This approach can prolong the patient’s recovery and drive up health care costs as patients are administered different therapies and clinically monitored for improvement. Treating patients with incorrect or unneeded antibiotics has largely contributed to the emergence of antibiotic-resistant organisms which are now becoming a serious threat to public health worldwide.
Common lower respiratory infections include:
- Pneumonia
- Hospital-Acquired Pneumonia (HAP)
- Hospital Community-Acquired Pneumonia (HCAP)
- Ventilator-Associated Pneumonia (VAP)
Our initial research strongly suggested a critical market need to improve and simplify the diagnosis of bacterial respiratory infections, particularly in the context of various types of pneumonia. Of critical importance is the fact that current tests appear to fall into two categories:
- Fast, minimally-invasive, but less accurate
- More accurate, but highly invasive and slow
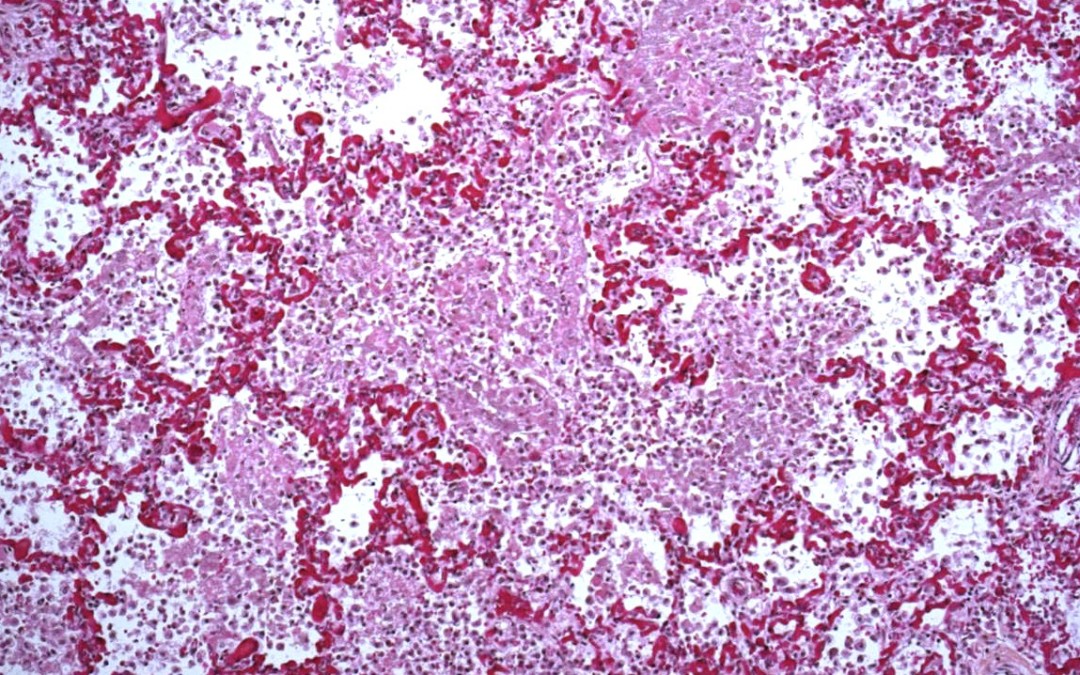
These include clinical history and observation, chest X-ray, blood tests, Tracheal Aspirates (TA) (taking fluid from the upper respiratory tract), and Broncho-Alveolar Lavage (BAL) (taking fluid from the lower respiratory tract). In each case of specimen collection, whether blood, TA, or BAL, the primary test is bacterial culture followed by pathology to determine the exact organisms present. Often the first line of treatment for pneumonia is immediate empiric therapy with broad spectrum antibiotics to provide the best odds for the patient’s full and fast recovery.
These therapies are often administered before any pathology results are available to specifically guide the use of antibiotics. This common practice is believed to contribute to the evolution of drug-resistant bacteria. The emergence of new, virulent, antibiotic-resistant strains such as Methicillin-Resistant Staphylococcus Aureus (MRSA) has created a sense of urgency in the medical community to improve diagnostic accuracy and targeted therapy. However, physicians today are forced to decide between the immediate needs of the single patient and the longer-term effects on public health. Nearly always, the immediate needs of the patient prevail.
Pseudomonas Aeruginosa and Staphylococcus Aureus/Methicillin-Resistant Staphylococcus Aureus bacteria, which cause most of the fatal pneumonias in America, create unique Volatile Organic Compounds (VOC) which can be measured in gas phase. Mass Spectrometry is the widely-acknowledge gold standard for the accurate detection of VOC’s and has been used extensively to characterize VOC’s in human exhaled breath. Applying this technology to a point-of-care breath test for infectious respiratory disease has the disruptive potential to substantially improve patient outcomes and public health while driving down the cost of care.
This test modality could deliver immediate results specific to the deep lower airway:
- Serve ambulatory and intubated (on mechanical ventilation) patients at the point of care
- Non-invasive
- No risk of infectious cross-contamination between patients
These results could be used to:
- Differentiate an exacerbation from a new infection in Cystic Fibrosis patients
- Help determine which COPD patients my need to be admitted to the hospital under suspicion of bacterial pneumonia
- Screen all patients entering the emergency room to determine any potential infectious threat they may pose to other patients
- Help establish the presence or absence of pneumonia in asymptomatic patients for record keeping in the event that a subsequent infection is deemed to be a Hospital Acquired Infection (HAI)
For all the promise of such a test, several key questions remain:
- What is the accuracy, sensitivity and reproducibility of MS in this application?
- Do PA and SA produce the same unique VOC’s in vivo as they do in vitro?
- Do they produce the same VOC’s in different lung environments?
- Do other benign bacteria produce the same VOC’s?
- Do VOC levels correlate to metabolic activity of the colony?
- Is increasing metabolic activity indicative of a causal effect between the existence of the colony and the disease process?
- Can these VOC’s be masked by much higher levels of other VOC’s in the breath?
Clinical Research Progress
These are difficult questions to answer and will require advanced tools and a sustained research commitment. This is the purview of the research community and we are honored to be able to support you. Two critical pieces of this effort with which we can help are:
- The need to selectively collect End Tidal Air, also known as Alveolar Air, to serve as the optimal matrix for relevant breath VOC’s
- The need to rapidly and accurately measure VOC’s at or near the point-of-care
We at Respiratory Research invite you to consider our vision for how this will be accomplished using a portable mass spectrometer and a disposable End Tidal Air Collector. See a short video outlining this vision and showing in real, practical terms how this technology would be deployed at the point-of-care. This system is available now for research use in the development of breath diagnostics and represents the best of our ability to support the research community in this critical endeavor.
Please contact us to discuss your research plans and needs. This research is vital to both sick patients and public health and we are committed to supporting the research community in this pursuit.